Welcome to my almost deep dive on BPD (borderline personality disorder, tragically not beautiful princess disorder).
This is part two of a little trilogy on personality disorders. I started this because of a discussion with my psychologist in which she said clinicians sometimes “lose curiosity” over what treatments could work after they’ve “decided” a patient has borderline personality (whether there’s an official diagnosis or not).
I wanted to unpack this but it was bigger than one post (and I had to do it over a few weeks because I needed so much time to procrastinate) so I’ve split it up. Part one, on what a personality is and what makes one disordered, can be read here.
There are heaps of personality disorders, and I don’t have the capacity or skill to unravel them all. I gave a brief overview of the different clusters in my first post, but in this part I’m going to unpack BPD specifically.
(Pls remember I am just a silly little guy with no training or expertise and also I don’t have the ability or capacity to fully explain everything to do with this complex disorder. That would take approx one trillion years and require a much better brain than I possess. These are just SOME of MY thoughts and research. But again, I am just a baby and I am very tired.)
what is bpd 👸
BPD is a personality disorder characterised by the following nine traits:
unstable self-image or sense of identity
intense and unstable interpersonal relationships
recurrent self-harm or suicidal behaviour, gestures or threats
chronic feelings of emptiness
emotional regulation issues (for example, quick, dramatic changes in mood; strong, overwhelming emotions)
self-damaging impulsivity (for example, substance abuse, reckless driving, binge eating, impulsive spending)
intense and inappropriate anger or difficulty controlling anger
fear of abandonment and frantic efforts to avoid real or perceived abandonment
stress-related paranoia or severe dissociation
According to the Diagnostic and Statistical Manual of Mental Disorders (DSM), to be diagnosed with BPD you need to show at least five of these traits and they need to be pervasive and enduring. That means there are 256 different combinations of symptoms that could result in diagnosis of BPD, so there is a huge spectrum of experiences that fit under this one label.
on the border of what? 🗺️
I think part of our misunderstanding of BPD comes from the diagnosis being murky as soon as we hear about it. Other personality disorders seem easier to clarify at face value (though not all of them!), using words like antisocial, paranoid, dependent, narcissistic. It gives us a hint from the very beginning. When we hear “borderline”, it’s confusing. On the borderline of what?
(In the UK and parts of Europe, BPD is more commonly called Emotionally Unstable Personality Disorder (EUPD). This started in the late 20th century as a way to focus on the symptoms of the disorder and to reduce stigma. I don’t know how I feel about this. It does exactly what it says on the tin, I guess??? But does “emotionally unstable” feed into the stereotype of being crazy and dangerous? Surely there’s something better?)
When the concept of borderline was first introduced in the 1930s, it was because patients were presenting with symptoms that seemed to be on the border of psychosis (disconnect from reality) and neurosis (anxiety, obsessions). It was often used against women who were “difficult” or seen as “untreatable”.
BPD was first recorded as a disorder in 1980. The name stuck, even as we learnt more and more about BPD and even though the symptoms were clarified.
what else could it be? 🕵️♀️
Historically there has been controversy and debate about the legitimacy of BPD as a diagnosis. Now, as we keep discovering more, some people with BPD and some clinicians have raised the following possibilities as alternatives:
(note: BPD is more commonly diagnosed in women than other genders and some of these possibilities try to explain that. The research on non-binary, gender queer and trans folks with BPD is limited, but my gut says they are maybe more likely to experience an invalidating environment, the “nurture” part of BPD development, so we should, like, research that??? )
BPD is actually neurodivergence (specifically autism and/or ADHD) presenting differently than we are used to seeing in cis men (AKA the norm for previous research). Currently, there’s an increase in people getting rediagnosed with ADHD or autism after being originally diagnosed with BPD.
BPD is actually a trauma disorder and just presents slightly differently than the current understanding of complex PTSD (trauma is not in the diagnostic criteria for BPD but is common, in varying degrees, in BPD patients). C-PTSD and BPD share very similar diagnostic criteria, though there are also some clear differences.
BPD is actually an attachment disorder. It could be brought on by trauma or emotional needs not being met in childhood. A lot of BPD symptoms are focused on difficulties with relationships, fear of abandonment, switching between devaluation and idealisation, sense of self and the need for external validation, which can all tie back to attachment. Though, again, trauma is not part of the diagnostic criteria for BPD.
Research in this area is ongoing. Our understanding of the brain and how it works is always developing.
For me, I felt such relief at getting diagnosed with BPD. It felt validating and explained my experience so well. So despite the debates and opinions, I draw the line, in regards to my experiences, there. For my own wellbeing. Other people will think differently and that’s cool too.
what causes bpd? 👩🔬
As with everything ever in the whole world, BPD is likely caused by a mix of nature and nurture.
Experiences you have at a young age can dramatically impact your later life—and I’m not just talking about significant trauma. Things like living in an invalidating environment, not getting your emotional needs met and having a particularly sensitive child with a parent who is not sensitive or aware of that sensitivity can hugely impact our attachment style, sense of self and understanding of interpersonal relationships.
In terms of biology, research has shown the following in people with BPD when compared to those without BPD:
A more active and reactive amygdala (a part of brain used to process emotions). This could help to explain the hyper-sensitivity and intense emotions many people with BPD experience.
Increased connectivity between the amygdala and other parts of the brain that help process emotions.
Decreased connectivity between the amygdala and the prefrontal cortex (a part of the brain used to control impulses and make decisions).
Differences in the thickness in the outer layer of the brain.
Differences in the amount of gray matter in the brain. Gray matter is made up of Important Brain Things that I don’t really understand but it is essential for processing information, memory and emotions.
A smaller hippocampus (involved in memory formation and managing emotions) that is more sensitive to stress and functions differently (some studies show it was more active and some studies showed it was less active, but either way, differences were noted.).
Differences in serotonin (helps with emotional regulation and impulse control) and dopamine (helps process pleasure, motivation and reward) transmitters.
Though more research is needed, there are clear signs of something going on in the brains of BPD baddies. Others being born with the same differences that then reacclimatise based on environment is a possibility too. I can’t understate how little we know about the brain!!! And how little I know!!!
stigma 🚫
There is SO much stigma around BPD. Everyone I know with BPD (there is so many of us, hi! I promise you know someone with BPD. Even if you don’t know you know them!) has personal experience of this.
People often think of BPD as attention-seeking, dangerous, manipulative and too difficult to deal with. We’re easily dismissed and written off as crazy, chronic and beyond help. BPD can be seen as flaw in someone’s character, not a mental illness.
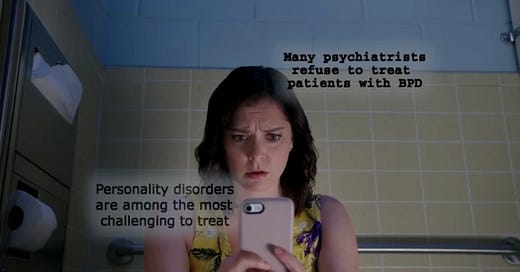
In studies on BPD stigma, mental health clinicians (!) reported feeling less empathy (!!) and more hostility (!!!) towards patients with BPD (!!!!!!!!). Some reported feeling pessimistic about treatment outcomes and that therefore it wasn’t worth treating them at all. Some clinicians will straight out refuse to treat BPD patients. Marsha Linehan, the creator of dialectical behavioural therapy (the therapy created specifically for BPD), has said that she tells clients not to disclose their BPD diagnosis during other health-related appointments as it will significantly impact their care.
Sometimes BPD is over-diagnosed as a catch-all for people who are chronically unwell and seen as difficult, especially in women. Some clinicians under-diagnose BPD to avoid opening up a world of stigma for a client who is already struggling.
BPD in popular culture hasn’t helped stigma and stereotypes either. The representation is limited but usually heavily criticised by those with a proper understanding of BPD.
In recent years, we saw Amber Heard’s potential diagnosis of BPD (it wasn’t confirmed, just speculated!!!) used as sure confirmation of her poor character and dangerous behaviours, and as a means to discredit what she was saying, in the court case between her and Johnny Depp. I don’t want to go back down this rabbit hole and I have a terrible memory. My point is that, regardless of facts and who did what, BPD was weaponised in a way that implied it was inherent evidence of her abuse. On top of this, the social media response was overwhelming and devastating and linked abuse and BPD constantly. It felt like almost everywhere there were damaging, hurtful conversations.
(Studies have shown people with BPD are more likely to be victims of crime than perpetrators; more likely to harm themselves physically than others; and are no more dangerous than those without BPD.)
Of course, some people with BPD will be abusive and manipulative and commit criminal offences, but so will millions of people who don’t have BPD. There are so many other factors that come into play there. And while people around someone with BPD may feel as thought they are being manipulated, it’s more likely that their loved one is using ineffective interpersonal skills to try to be understood, show their pain and avoid abandonment, rather than intentionally manipulating them. (Which is not to discount the struggle of supporting someone with complex mental health needs. It’s super tough and still hurtful, regardless of intent. It’s just different to work through when you see it as ineffective communication rather than intentional manipulation and coercion.)
The stigma and stereotyping around BPD restricts treatment access, decreases positive outcomes, increases suffering and ultimately kills people. If people can’t get the help they need from the mental health clinicians (you know, the people who are specifically supposed to help them), then what?????
(And the worst part is the BPD can be effectively treated and managed using intensive DBT!!! A therapy designed specifically for treating BPD!!! Some people even go into remission and no longer met the diagnostic criteria!!! Another terrible part is how accessible accurate and helpful information and research is online!!! You can disprove stereotypes so easily!!!)
My biggest and most confusing sticking point here isn’t even related specifically to BPD: why is it so hard to treat people with even just a tiny little bit of empathy?
If people with BPD have to work so hard to remain dialectical and grounded, then people without BPD should have to put in, like, just a few seconds of critical thinking, empathy, compassion and fact-checking. As a treat.
Next time I am going to write about my experience of BPD, stigma and the mental health system in New Zealand. Can’t wait!!!!!!!!!!!!!!